Search for tests or checkups
SupportUnderstanding Impaired Fasting Glucose: Definition, Causes and Symptoms

The changing lifestyle and unhealthy habits of individuals in India have led to an increase in diseases. One of the most prominent examples of this is the increase in the prevalence of type 2 diabetes mellitus (T2DM) in the urban regions of India from 2% in the 1970s to 20% in 2018. The upward creep of T2DM could probably be explained by the fact that prediabetes (a precursor to diabetes), characterised by impaired fasting glucose, often goes unnoticed due to lack of symptoms. Early identification of impaired fasting glucose (levels >100 mg/dL and <126 mg/dL) is essential for regulating impaired fasting blood sugar and preventing T2DM. Once T2DM develops, it becomes irreversible. To prevent that from occurring, let's understand the concept of impaired fasting glucose and explore its causes, risk factors, methods of diagnosis, symptoms, and the significance of regular monitoring and follow-up in managing this condition.
What Does Impaired Fasting Glucose Mean?
Impaired fasting glucose denotes a higher level of blood glucose in a person who has been fasting for 8-12 hours. These blood glucose levels are higher than normal but lower than those in a person with T2DM. Impaired fasting glucose means fasting plasma glucose levels ranging from 100-126 mg/dL.
Causes of Impaired Fasting Glucose
The exact impaired fasting glucose causes are unknown but genetic mutations and improper functioning of the pancreas can lead to impaired fasting glucose. There is a multitude of risk factors that are associated with impaired fasting glucose, a few of which are listed below:
- Obesity
- Less physical activity
- Age
- Family history
- Smoking
- Taking medications such as certain HIV medicines or steroids
- Other health conditions: Certain medical conditions, such as polycystic ovary syndrome (PCOS) and non-alcoholic fatty liver disease (NAFLD) are associated with an increased risk of impaired fasting glucose.
Symptoms of Impaired Fasting Glucose
People with impaired fasting glucose have a higher risk of developing T2DM and other health complications. Here are some common symptoms of impaired fasting glucose:
- Vision changes that can progress to retinopathy associated with diabetes
- Acanthosis nigricans or darkening of the skin at the sides or back of the neck or in the armpit
- Small skin growths called skin tags
It's important to note that many people with impaired fasting glucose may not experience noticeable symptoms, which is why regular check-ups and blood tests are crucial for early detection and management.
Diagnosing Impaired Fasting Glucose
For impaired fasting glucose diagnosis, you must follow these simple steps:
- Fasting Blood Sugar (FBS) Test: This test measures blood glucose level after an overnight fast of at least 8 hours. The normal fasting blood glucose level is typically between 70 to 100 mg/dL (3.9 to 5.5 mmol/L). Fasting blood glucose levels between 100 to 125 mg/dL (5.6 to 6.9 mmol/L) are indicative of impaired fasting glucose.
- Confirmatory Testing: If the initial FPG test shows elevated glucose levels, your healthcare provider may recommend a repeat test on a separate day to confirm the diagnosis.
- Oral Glucose Tolerance Test (OGTT): In some cases, an oral glucose tolerance test may be used to diagnose impaired fasting glucose. This test involves fasting overnight and then consuming a glucose-containing drink (glucose challenge test). Blood glucose levels are measured at specific intervals to assess how well your body clears glucose from your bloodstream.
If you suspect you have impaired fasting glucose or are at risk of developing prediabetes, it is crucial to consult a healthcare professional for proper evaluation and guidance.
The Importance of Regular Monitoring and Follow-up
Impaired fasting glucose means a person does not have T2DM yet but is at a higher risk of developing it. The condition of impaired fasting glucose is reversible and a crucial component of impaired fasting glucose treatment is early identification and regular monitoring and follow-up to prevent T2DM, which is irreversible.
The steps to be followed for monitoring of impaired fasting glucose are as follows:
- Monitor blood glucose levels in the fasting state and 2 hours after meals at least once a month and with increased frequency if values are not within the target range.
- Check HbA1c levels every 6-12 months. If HbA1c levels are not in the desired target range, an every-3-month check is advisable.
- Get yourself checked by a doctor at least once every 3 months.
- Get foot examinations done at every visit to your doctor and educate yourself on foot care.
- Get screening done for long-term complications of diabetes such as retinopathy, nephropathy, neuropathy, peripheral vascular disease (PVD), and coronary artery disease (CAD) at least once a year, with more frequent screening if necessary.
- Focus on optimising your weight, waist circumference, blood pressure, and lipid levels.
Your healthcare team can assist you in choosing the best monitoring method and provide guidance on the frequency and timing of checks for impaired fasting glucose.
Follow-up: If your fasting glucose is in the normal range (<100 mg/dL), a follow-up visit every three years can be scheduled; however, if your fasting glucose is not in the normal range, then annual follow-up visits for monitoring is necessary.
Book Online Appointment to Check Impaired Glucose Range With Orange Health Labs
Your doctor will advise tests for the regular monitoring of blood glucose for early detection and prevention of T2DM. Let’s see how this can be done with the help of a convenient doorstep service:
- Log into our website
- Submit your details.
- In just 60 minutes, our highly trained professionals will be at your doorstep for sample collection.
FBS Test in Bangalore | FBS Test in Mumbai | FBS Test in Hyderabad | FBS Test in Noida | FBS Test in Gurgaon | FBS Test in Delhi | FBS Test in Faridabad
Individuals diagnosed with diabetes can support their healthcare providers by maintaining comprehensive records of their blood glucose levels and pertinent details, such as alterations in physical activity, medication usage, or sleep patterns. Moreover, they should actively inquire with their doctors regarding dietary and lifestyle practices that may impact their blood glucose levels.
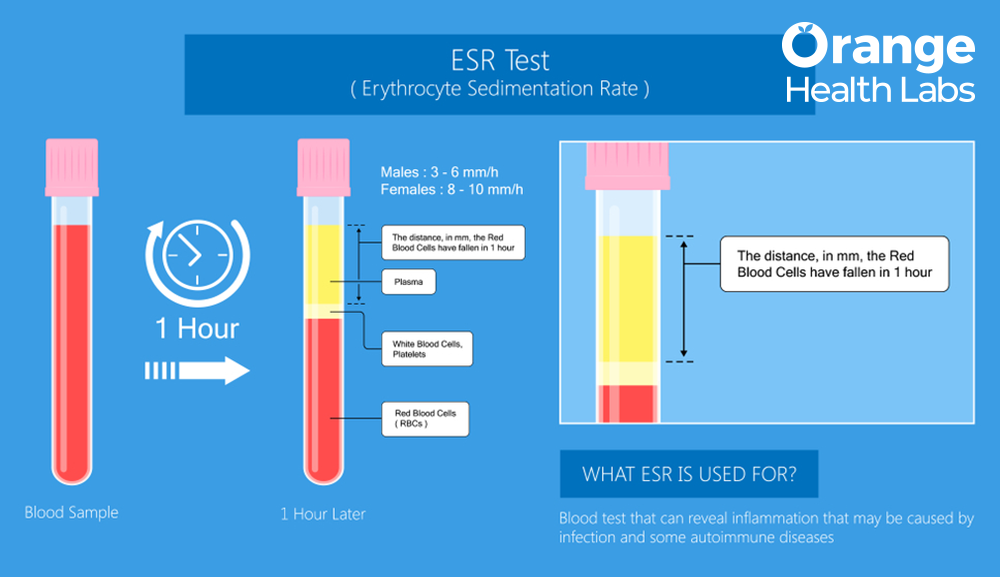
High Erythrocyte Sedimentation Rate (ESR): Unraveling Causes, Symptoms, and Significance

Managing Fasting Blood Sugar Levels: Highs, Lows, and Healthy Range